With the invention of antibiotics in 1928, human history was modified endlessly. Infectious diseases resembling pneumonia, tuberculosis, and sepsis were common and deadly until penicillin made them treatable. Surgical procedures that when carried a high risk of infection became safer and more routine. Antibiotics marked a triumphant moment in science that transformed medical practice and saved countless lives.
But antibiotics have a drawback: If used excessively, bacteria can develop resistance to those drugs. The World Health Organization estimated that these superbugs were caused 1.27 million deaths worldwide in 2019 and is more likely to change into an increasing threat to global public health in the approaching years.
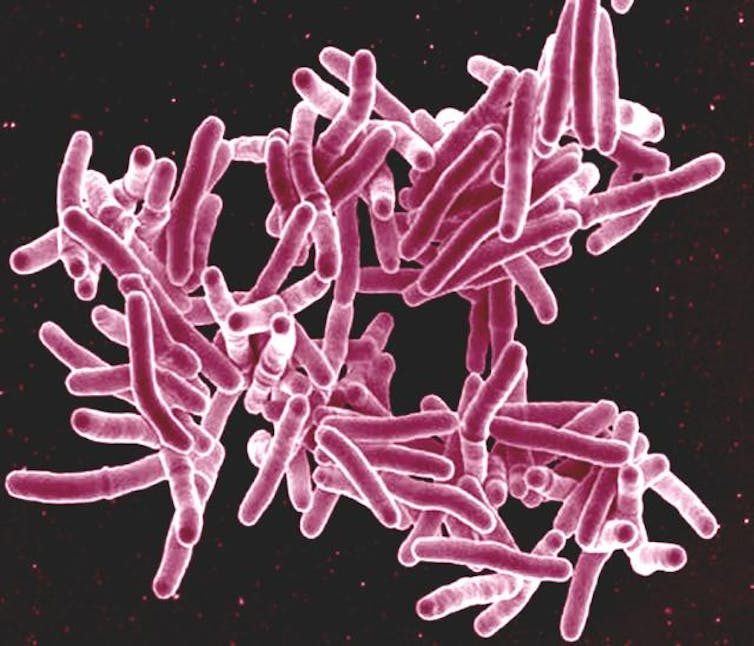
NIAID/Flickr, CC BY
New discoveries are helping scientists meet this challenge in modern ways. Studies have found this almost 1 / 4 Medications that will not be normally prescribed as antibiotics, resembling drugs used to treat cancer, diabetes and depression, can kill bacteria at doses normally prescribed to people.
Understanding the mechanisms underlying the toxicity of certain drugs to bacteria could have far-reaching implications for medicine. If non-antibiotic drugs attack bacteria in other ways than standard antibiotics, they might function clues for developing latest antibiotics. However, if non-antibiotics kill bacteria in an identical method to known antibiotics, their prolonged use, for instance within the treatment of chronic diseases, could inadvertently promote antibiotic resistance.
In our recently published research resultsMy colleagues and I actually have developed a brand new machine learning method that not only identifies how non-antibiotics kill bacteria, but may help find latest bacterial targets for antibiotics.
New ways to kill bacteria
Many scientists and doctors world wide are addressing the issue of drug resistance. including me and my colleagues in Mitchell Lab at UMass Chan Medical School. We use the genetics of bacteria to check which mutations make bacteria more resistant or sensitive to drugs.
When my team and I learned in regards to the widespread antibacterial effects of non-antibiotics, we were intrigued by the challenge it presented: determining how these drugs kill bacteria.
To answer this query, I used a genetic screening technique that my colleagues recently developed to check how this is finished Cancer drugs goal bacteria. This method identifies which specific genes and cellular processes change when bacteria mutate. By observing how these changes affect bacterial survival, researchers can draw conclusions in regards to the mechanisms by which these drugs kill bacteria.
I actually have collected and analyzed nearly 2 million cases of toxicity between 200 drugs and hundreds of mutant bacteria. Using a machine learning algorithm I developed Derive similarities between different medicationsI grouped the drugs right into a network based on how they affected the mutated bacteria.
My maps clearly showed that known antibiotics were present lined up closely together through their known classes of killing mechanisms. For example, all antibiotics that concentrate on the cell wall – the thick protective layer that surrounds bacterial cells – have been grouped together and well separated from antibiotics that interfere with bacterial DNA replication.
Interestingly, after I added non-antibiotic drugs to my evaluation, they formed separate centers from antibiotics. This indicates that non-antibiotic and antibiotic drugs have different methods of killing bacterial cells. Although these groupings don’t reveal how each drug specifically kills antibiotics, they do show that the grouped agents likely work in similar ways.
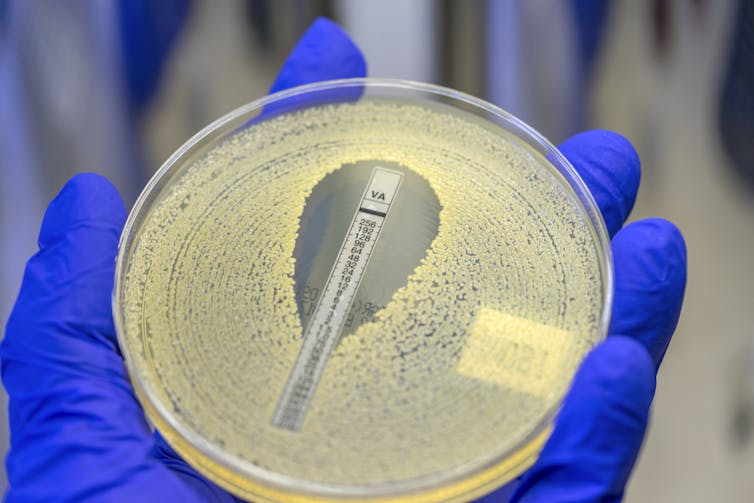
Rodolfo Parulan Jr./Moment via Getty Images
The final piece of the puzzle – whether we could find latest drug targets in bacteria to kill them – comes from my colleague’s research Carmen Lee. She grew tons of of generations of bacteria exposed to varied non-antibiotic drugs commonly prescribed to treat anxiety, parasitic infections and cancer. By sequencing the genomes of bacteria which have evolved and adapted to the presence of those drugs, we were in a position to pinpoint the particular bacterial protein Triclabendazole – a drug used to treat parasitic infections – goals to kill the bacteria. Importantly, current antibiotics typically don’t attack this protein.
In addition, we found that two other non-antibiotics that use an identical mechanism to triclabendazole also goal the identical protein. This demonstrated the facility of my drug similarity maps to discover drugs with similar killing mechanisms, even when that mechanism was still unknown.
Assisting in the invention of antibiotics
Our results open up quite a few opportunities for researchers to check how nonantibiotic drugs work otherwise than standard antibiotics. Our drug mapping and testing method also has the potential to handle a critical bottleneck in antibiotic development.
The search for brand new antibiotics typically requires the use of serious resources to check hundreds of chemicals that kill bacteria and determine how they work. Most of those chemicals act similarly to existing antibiotics and are discarded.
Our work shows that combining genetic screening and machine learning can assist uncover the chemical needle within the haystack that may kill bacteria in ways in which researchers haven’t yet exploited. There are other ways to kill bacteria that we haven't used yet, and there are still ways to combat the specter of bacterial infections and antibiotic resistance.
image credit : theconversation.com


















Leave a Reply