How did your heart come to be? What caused your first heartbeat? To date, the mechanisms of human heart development remain unclear.
Researchers know that's what the center is first organ to be fully functional within the growing human embryo. It begins as an easy tube that begins pumping blood from the fourth week of pregnancy. In the ninth week the center is fully formed. The heart is crucial to early development because it provides essential nutrients to the whole developing fetus.
However, as a result of its early formation, the center is exposed over an extended time period to substances that a pregnant person could come into contact with, resembling: Medication or pollutants. This could possibly be a significant reason why congenital heart defects are essentially the most common variety of birth defect in humans over 1 in 100 births worldwide.
Traditionally, scientists have used animal and cell models to review heart development and disease. However, researchers have been unable to develop a cure for congenital heart defects, partly because these models are unable to capture the disease Complexity of the human heart. For ethical reasons, the usage of human embryos for these studies is out of the query.
To help researchers study heart development and complications in pregnancy, our team from Biomedical engineers And Cardiovascular scientist I've spent the previous couple of years attempting to create the subsequent smartest thing: Mini human hearts within the laboratory.
Human cardiac organoids
Organoids are complex three-dimensional cell structures that replicate key facets of the structure and performance of a particular organ in your body. Although organoids aren’t (yet) fully synthetic, functioning organs, they still have an incredible ability to mimic vital facets of physiology and disease within the laboratory.
We made our heart organoids from a variety of cell called a pluripotent stem cell. Although the usage of these cells in research was once controversial as they were originally obtained from human embryos, today this is not any longer an issue as they will be produced by any adult. Pluripotent stem cells have the potential to turn into any variety of cell within the body. This signifies that cells from almost any a part of your body – typically blood or skin cells – will be converted into your personal stem cells to grow your personal mini heart.
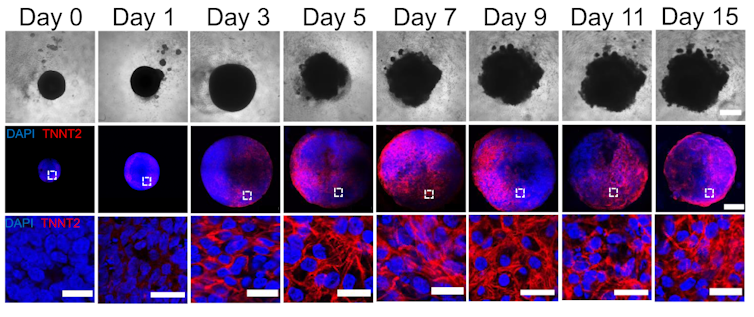
Jonathan R. Lewis-Israel et al. 2021/Nature Communication, CC BY-SA
By manipulating the flexibility of pluripotent stem cells to remodel into any variety of cell within the body, we are able to led these cells to turn out to be heart cells. The cells were capable of organize themselves and recreate the most important stages of human heart development while pregnant. Our heart organoids have blood vessels and all cell types present in the human heart, resembling cardiomyocytes and pacemaker cells, giving them a bonus over 2D cell models. Furthermore, the electrophysiology and bioenergetics of those cardiac organoids are very just like human embryonic hearts in a way that just isn’t the case in animal models.
Our heart organoids beat like the center of a tiny baby, but are smaller than a grain of rice.
Pregnancy and the fetal heart
One area we’re exploring with our heart organoids is maternal and fetal heart health. Maternal aspects resembling diabetes, hypertension or depression may increase the chance of heart disease in newborns. By studying conditions that increase the chance of congenital heart disease, the incidence of heart problems will be prevented and reduced worldwide.
Using cardiac organoids, we are able to mimic these maternal environments and simulate how they influence fetal heart development. For example, we used heart organoids to indicate that diabetes, a quite common disease, increases the chance of Heart disease in embryos. Compared to heart organoids created under healthy conditions, minihearts exposed to diabetic diseases developed cardiac abnormalities like human fetuses and newborns with diabetic cardiomyopathy.
Our study found that diabetes-related cardiac developmental disorders are likely brought on by an imbalance of omega-3 fatty acids, the constructing blocks of cell membranes and signaling molecules. However, supplementation with omega-3 fatty acids could also be possible partially restore this imbalance and forestall diabetes-related congenital heart defects.
Drug safety while pregnant
The medications that pregnant women take can have significant health effects on each the parents and the fetus. Medications approved to be used while pregnant aren’t all the time secure because they’re sufficient Testing is complicated. Ethical concerns limit working with human biological material, researchers say left with animal models that can’t replicate human physiology accurately enough.
Testing drugs on human heart organoids allows researchers to higher study and predict possible harmful effects while pregnant. One example is ondansetron (Zofran), a medicine often prescribed to forestall nausea and vomiting while pregnant. Although it was linked to 1 increased risk of congenital heart defectswhether it causes the disease has not been confirmed.
We showed that Cardiac organoids exposed to ondansetron had impaired ventricular cell development and performance, just like that seen in neonates exposed to ondansetron. Our results provide data which will help update clinical guidelines for the usage of the drug.

Fiordaliso/Moment via Getty Images
Another example concerns taking antidepressants while pregnant, which is related to a medical condition increased risk of congenital heart defects. Selective serotonin reuptake inhibitors, or SSRIs, essentially the most commonly prescribed antidepressants for pregnant women, work Increasing the supply of serotonin within the body. Serotonin is a very important molecule in heart development. Maternal serotonin, together with antidepressants, easily travels to the embryo and alters serotonin levels within the developing heart.
In the longer term, we plan to reveal cardiac organoids to antidepressants and study their effects on the incidence of congenital heart defects. The results of this research on human heart organoids may additionally provide recommendations for drug substitute or repurposing.
Heart organoids have the potential to assist scientists study the formation of the human heart and the event of disease in additional detail. In the sector of medical innovation, we consider that human heart organoids grown from stem cells hold the very best promise for a healthier future.
image credit : theconversation.com

















Leave a Reply