An easy difference within the genetic code — two X chromosomes versus one X chromosome and one Y chromosome — can result in big differences in heart disease. It seems that these genetic differences affect greater than just the sex organs and gender assigned at birth – they fundamentally change the best way heart problems develops and occurs.
While gender influences the mechanisms underlying the event of heart problems, gender plays a job in how healthcare providers recognize and treat it. Sex refers to biological characteristics corresponding to genetics, hormones, anatomy and physiology Gender refers to social, psychological and cultural constructs. women are more more likely to die after a primary heart attack or stroke than men. The probability can also be higher in women additional or different heart attack symptoms that transcend chest pain, corresponding to nausea, jaw pain, dizziness and fatigue. It is commonly difficult to completely distinguish the influence of sex on heart problems outcomes from the influences of gender.
While women who haven’t yet reached menopause have a lower risk of heart problems than men, their cardiovascular risk is lower accelerates dramatically after menopause. If a girl also has type 2 diabetes, her risk of heart attack increases equivalent to that of meneven when the girl with diabetes has not yet undergone menopause. More data are needed to higher understand differences in heart problems risk non-binary and transgender patients.
Despite these differences, one thing is similar: heart attacks, strokes and other types of heart problems are the identical thing commonest reason for death for all people, no matter sex or gender.
We are researchers that cope with women's health and the best way heart problems occurs develops and presents itself otherwise in men and women. Our work has identified an urgent must update medical guidelines with gender-specific approaches to diagnosis and treatment to attain this Improving health outcomes for all.
Sex differences in heart disease
The reasons for this Gender and gender differences in cardiovascular diseases should not fully known. The different biological effects of gender, corresponding to hormonal and genetic aspects, in comparison with gender, corresponding to social, cultural and psychological aspects, are also not clearly differentiated.
What researchers do know is that the collected evidence supports what good heart care should appear like for girls in comparison with men has as many holes as Swiss cheese. Medical evidence for the treatment of heart problems often comes from studies that excluded women, as until then women had largely not been included in scientific research NIH Revitalization Act of 1993. For example, current guidelines for treating cardiovascular risk aspects corresponding to hypertension apply based totally on data from men. This is despite evidence that differences in the best way heart problems occurs cause women to experience heart problems otherwise.

FG Trade Latin/E+ via Getty Images
In addition to the gender differences implicit gender bias amongst providers and gender social norms amongst patients cause doctors to underestimate the danger of cardiac events in women in comparison with men. These biases play a job in why women die from cardiac events more often than men. For example, in patients with symptoms bordering on heart problems, doctors are inclined to order arterial imaging more aggressively in men than in women. One study partially linked this tendency to order less aggressive tests for girls to a Gender bias that men are more willing to take risks than women.
In a study of about 3,000 patients who had recently suffered a heart attack, women were less likely than men to consider this Symptoms of a heart attack were resulting from heart disease. In addition, most girls have no idea that it’s heart problems No. 1 reason for death in women. Overall, women's misperceptions about their very own risk can prevent them from searching for medical attention to judge possible symptoms of a heart attack or stroke.
For women of color, these problems are further exacerbated. Lack of access to healthcare and extra challenges promote health inequalities amongst underrepresented racial and ethnic minorities.
Sex difference in heart disease
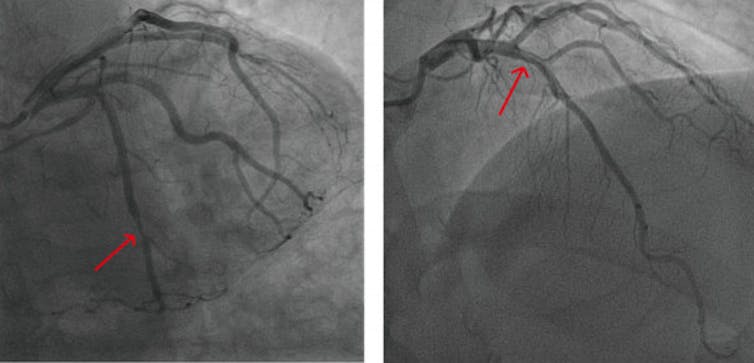
Cardiovascular disease looks physically different in men and women, particularly resulting from the plaque buildup on artery partitions that contributes to the disease.
women have fewer cholesterol crystals and fewer calcium deposits in arterial plaque than men. Physiological differences within the smallest blood vessels Heart nutrition also plays a job in cardiovascular outcomes.
Women are more likely than men to suffer from heart problems, which manifests itself in the shape of several narrowed arteries that should not completely “clogged”. This results in chest pain because blood flow can’t be increased enough to fulfill the upper oxygen demands brought on by exercise, just like low blood pressure. Flow shower head. When chest pain occurs in this manner, doctors call this condition Ischemia and no obstructive coronary arteries. In comparison, men usually tend to have a “clogged” artery in a concentrated area that could be opened with a stent or heart bypass surgery. Options for multiple narrowed arteries lag behind treatment options for typical “clogged” arteries, putting women at a drawback.
Zhao and Gong 2023/Mathematical Life Sciences and Engineering
In addition, within the early stages of a heart attack, levels of blood markers that indicate damage to the guts are increased are lower in women than in men. This may result in the next rate of missed diagnosis of coronary heart disease in women in comparison with men.
The reasons for these differences should not entirely clear. Some possible aspects These include differences in arterial plaque composition, which make plaque more more likely to rupture or rupture in men and plaque more more likely to erode in women. Women have it too lower heart mass and smaller arteries than men, even after accounting for body size.
Reducing gender differences
All too often, women with symptoms of heart problems are turned away from the doctor's office due to the gender bias that claims “women don't get heart disease.”
Considering different symptoms of heart problems depending on sex and gender could help doctors higher look after all patients.
One way the rubber is moving is thru higher approaches to diagnosing heart attacks in men and women. In particular, when diagnosing heart attacks, gender-specific limits are used for blood tests that measure heart damage – so-called highly sensitive troponin tests – may improve their accuracyThis reduces the variety of missed or false-negative diagnoses in women while reducing the variety of over-diagnoses or false-positive leads to men.
The heads of our research laboratory, Employees and other internationally recognized research colleagues – a few of whom collaborate with us Ludeman Family Center for Women's Health Research on the University of Colorado Anschutz Medical Campus – will proceed this vital work to shut this gender gap in healthcare. Research on this area It is critical to make clear ways physicians can higher manage gender-specific symptoms and advance tailored treatments.
The The Biden administration's latest executive order Funding women's health research paves the best way for research that goes beyond simply understanding the causes of sex differences in heart problems. Developing and testing appropriate treatment approaches for every patient may also help improve the health of everyone.
image credit : theconversation.com
















Leave a Reply