Infectious or chronic diseases akin to long COVID, Alzheimer's disease and traumatic brain injuries may cause inflammation within the brain. or neuroinflammationthis weakens the muscles. Although scientists are aware of this connection between inflammation and muscle weakness, the molecules and processes involved remain unclear.
In our research, our team by neuroscientists and biologists revealed hidden conversation between brain and muscles that trigger muscle fatigue and possible treatment options.
Neuroinflammation and muscle fatigue
Neuroinflammation occurs when your central nervous system—brain and spine—prompts its own immune system to guard itself from infection, toxins, neurodegeneration, and traumatic injury. Neuroinflammatory reactions occur primarily within the brain. But for unknown reasons, patients also experience many symptoms outside the central nervous system, akin to: B. debilitating fatigue and muscle pain.
To solve this puzzle, we examined brain inflammation related to three different diseases: bacterial infection in -induced meningitis; viral infection in COVID-19; and neurodegeneration in Alzheimer's disease. We then analyzed how these immune changes affect muscle performance.
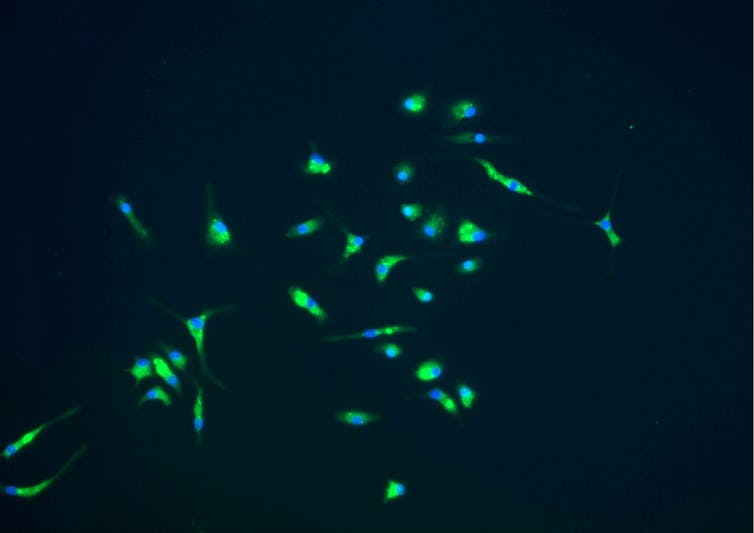
We measured immune changes within the brains of fruit flies and mice infected with live bacteria, viral proteins, or neurotoxic proteins. After the initial buildup of toxic molecules within the brain, which normally increase in response to stresses akin to infections, the brain produces large amounts of Cytokines – Chemicals that activate the immune system – released into the body. When these cytokines travel to the muscles, they trigger a series of chemical reactions disrupts the power the ability plant of the cells – the mitochondria – to generate energy.
National Institute of Allergy and Infectious Diseases/NIH via Flickr
Although the results of these immune changes doesn’t appear to wreck muscle fibers, it does result in fatigue. When we measured the muscle performance of those animals after giving them treatments to offset the results of immune activation, we found that each flies and mice moved significantly less in response to manual or mechanical stimuli in comparison with those that weren’t infected. This suggested that the animals had reduced endurance.
Conversations between brain and muscle
Our results suggest that muscle fatigue resulting from infection or chronic disease is brought on by a. is caused Communication path from brain to muscle This expends energy within the muscles without affecting their structure or integrity. Unlike traditional explanations for muscle dysfunction that deal with causes outside the brain, akin to: B. Damage to the muscle fibers, this path leads on to fatigue.
Since then, it has been the important thing cytokine involved in brain-muscle communication preserved throughout evolution Across species, we imagine this pathway may represent a universal mechanism that the brain uses to harness and redistribute energy to fight infection.
Because now we have only studied the brain-muscle axis in simplified models, we have no idea whether it applies to more complex diseases akin to fibromyalgia or chronic fatigue syndrome. We also don't know the way impaired energy production within the muscles is expounded to impaired energy production within the brain.
In addition, the brain-muscle axis works through quite a few interconnected steps. However, the precise mechanism of this communication and the possible involvement of other cytokines are unknown.
Muscle fatigue is common in all diseases
Muscle weakness and fatigue are the result common symptoms in several diseasesstarting from bacterial and viral infections to chronic diseases and neurodegenerative diseases. These symptoms are distressing and affect the standard of lifetime of thousands and thousands of individuals worldwide.
For example, many of the 65 million people on the earth struggle with it long COVID Experience Prevent fatigue Duration from months to years.
Likewise, reduced muscle strength is a standard symptom of Early stage Alzheimer's diseasea condition that no less than affects 50 million people worldwide.
A greater understanding of how neuroinflammation causes muscle fatigue may result in possible treatments that improve muscle function.
New treatments on the horizon
Our work suggests that targeting the brain-muscle axis could provide latest treatment strategies for muscle fatigue.
We are currently testing neutralizing antibodies – Proteins that bind to cytokines and inhibit their function – in mice with neuroinflammation. These FDA-approved treatments specifically goal the cytokines secreted by the brain and forestall signal transmission to the muscles. We are desirous about checking out which neutralizing antibodies or combos of antibodies prevent muscle fatigue in mice.
We are also planning an extended COVID clinical trial to evaluate cytokine levels in patients. It is unclear whether other COVID-19 proteins can even trigger neuroinflammation and muscle fatigue. Recent evidence suggests there could also be a connection to long-COVID remaining virus particles in multiple organs, including the brain, even months after infection. However, it’s uncertain whether and the way this is expounded to the high values Cytokines seen in long COVID.
If further developed, targeting the brain-muscle axis might be a useful treatment for people affected by long-COVID and other diseases that cause brain inflammation.
image credit : theconversation.com

















Leave a Reply