The practice of medication has undergone an incredible, if incomplete, transformation over the past 50 yearsand is steadily moving from a field based totally on expert opinion and the anecdotal experience of individual clinicians to a proper scientific discipline.
The emergence of evidence-based medicine This meant that doctors identified probably the most effective treatment options for his or her patients based on high-quality evaluations of the most recent research. Now, Precision medicine allows providers to make use of a patient's individual genetic, environmental and clinical information to further personalize their care.
The potential advantages of precision medicine also bring recent challenges. Importantly, the quantity and complexity of information available for every patient is rapidly increasing. How can doctors determine which data is helpful for a selected patient? What is probably the most effective strategy to interpret the info to pick out the perfect treatment?
These are precisely the challenges Computer scientists like me which we’re working to resolve. Working with experts in genetics, medicine, and environmental sciences, my colleagues and I develop computer-based systems that usually use artificial intelligence to assist clinicians integrate a wide range of complex patient data to make the perfect care decisions.
The rise of evidence-based medicine
Like recently like within the Nineteen SeventiesClinical decisions were based totally on expert opinion, anecdotal experience and theories about disease mechanisms, which were often not supported by empirical research. At the time, some pioneering researchers argued that clinical decision-making needs to be based on the perfect available evidence. In the Nineties the term evidence-based medicine was introduced to explain the discipline of integrating research and clinical expertise in making decisions about patient care.
The foundation of evidence-based medicine is a Hierarchy of evidence quality This determines what forms of information physicians should depend on most when making treatment decisions.
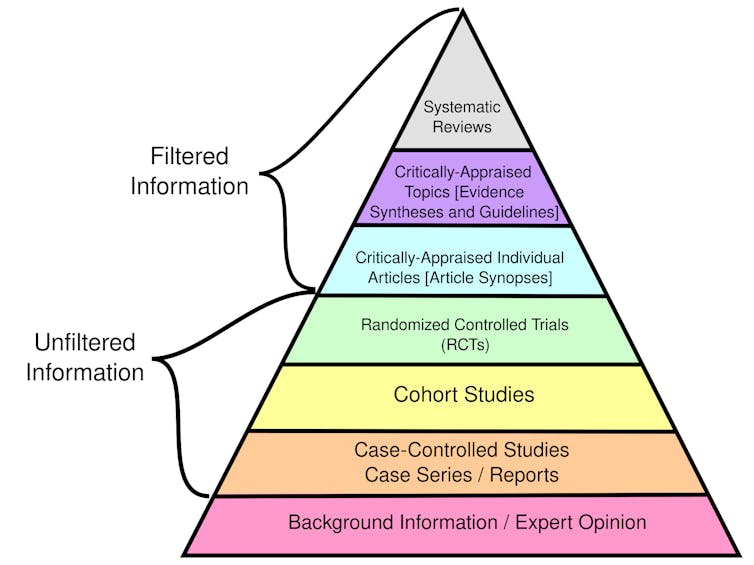
CFCF/Wikimedia Commons, CC BY-SA
Randomized controlled trials Randomly assign participants to different groups to receive either an experimental treatment or a placebo. These studies, also called clinical trials, are considered the perfect individual sources of evidence because they permit researchers to check the effectiveness of treatment with minimal bias by ensuring that the groups are similar.
Observational studiesSome studies, resembling cohort and case-control studies, concentrate on the health outcomes of a gaggle of participants without researcher intervention. Although these studies are utilized in evidence-based medicine, they’re considered weaker than clinical trials because they don’t control for potential confounding aspects and bias.
Overall, systematic reviews that summarize the outcomes of multiple research studies provide the very best quality evidence. In contrast, individual case reports detailing a single person's experiences are weak evidence because they might not apply to a broader population. Personal reports and expert opinions alone are usually not supported by empirical data.
In practice, physicians can use the framework of evidence-based medicine to formulate a selected clinical query about their patient that may be clearly answered by reviewing the perfect available research. For example, a health care provider might ask whether statins could be more practical than eating regimen and exercise in lowering LDL cholesterol in a 50-year-old man with no other risk aspects. By integrating evidence, patient preferences and their very own expertise, they’ll develop diagnoses and treatment plans.
As you would possibly expect, collecting and compiling all of the evidence generally is a laborious process. As a result, physicians and patients often depend on clinical guidelines developed by Third resembling the American Medical Association, the National Institutes of Health and the World Health Organization. These guidelines provide recommendations and standards of care based on a scientific and thorough assessment of obtainable research.
Beginning of precision medicine
At in regards to the same time that evidence-based medicine was gaining traction, two other transformative developments in science and healthcare were underway. These advances would result in the emergence of Precision medicinethat uses patient-specific information to tailor health care decisions to every person.
The first was this Human genome projectwhich officially began in 1990 and was accomplished in 2003. The goal was to create a reference map of human DNA, or the genetic information that cells use to operate and survive.
This map of the human genome allowed scientists to find genes linked to 1000’s of rare diseases, understand why people respond in a different way to the identical drug, and discover mutations in tumors that may be targeted with specific treatments. Doctors are increasingly analyzing a patient's DNA to discover genetic variations that influence their treatment.
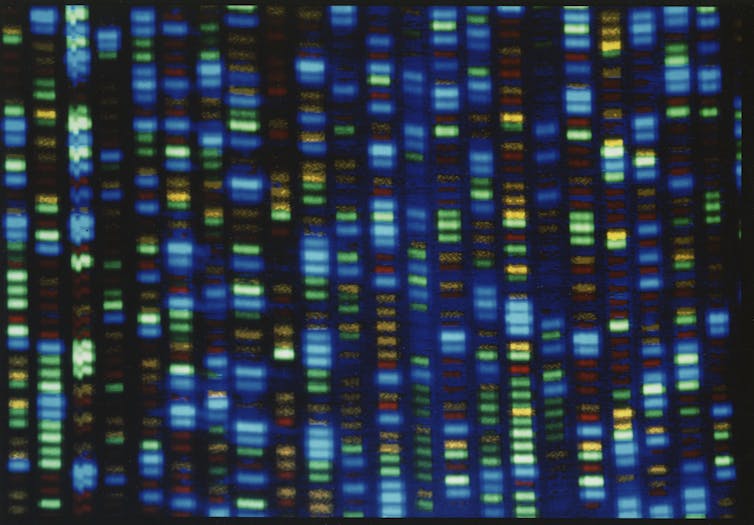
National Institute for Human Genome Research/Flickr
The second was the event of electronic medical records to store the patient's medical history. Although researchers had been conducting pilot studies on digital health records for several years, the event of industry standards for electronic health records didn’t begin until the late Eighties. Acceptance only became widespread after 2009 American Recovery and Reinvestment Act.
Electronic medical records enable scientists to conduct large-scale studies of the relationships between genetic variants and observable characteristics that influence precision medicine. By storing data in an organized digital format, researchers also can use these patient records to coach AI models to be used in medical practice.
More data, more AI, more precision
On the surface, the thought of using patient health information to personalize care isn’t recent. For example, the running thing Framingham Heart Studywhich began in 1948, provided a mathematical model for estimating a patient's risk of coronary heart disease based on their individual health information reasonably than the typical population risk.
However, a fundamental difference between efforts to personalize medicine now and before the Human Genome Project and electronic medical records is that the mental capability is required to research the quantity and complexity of individual patient data available today far exceeds that of the human brain. Each person has tons of of genetic variants, tons of to 1000’s of environmental exposures, and a clinical history that may include quite a few physiological measurements, laboratory values, and imaging results. In my team's ongoing work, we’re developing the AI models Recognizing sepsis in infants Use dozens of input variables, many updated hourly.
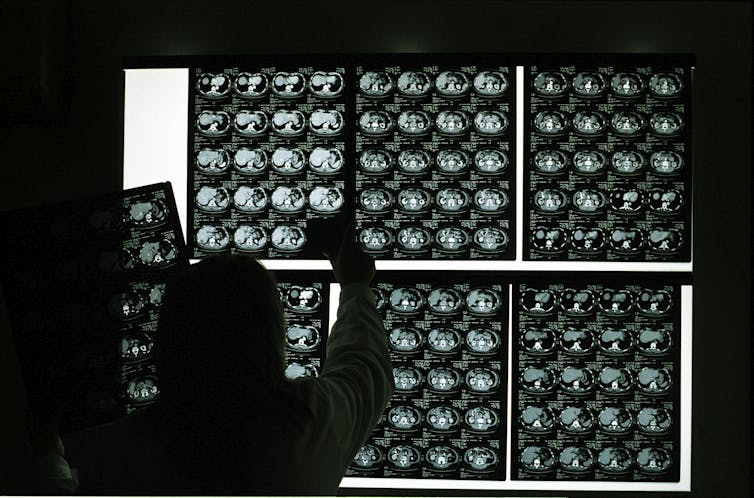
Marco Vacca/Photographer's Choice RF via Getty Images
Researchers like me are using AI to develop tools that help clinicians analyze all this data to tailor diagnoses and treatment plans to every individual. For example, some genes may influence how well certain medications work in several patients. Although genetic testing can reveal a few of these characteristics, it isn’t yet possible to screen every patient resulting from cost. Instead, AI systems can do that Analyze a patient's medical history to predict whether genetic testing will likely be of profit based on the likelihood of being prescribed a drug known to be influenced by genetic aspects.
Another example is diagnosis rare diseasesor diseases that affect fewer than 200,000 people within the United States. Diagnosis could be very difficult because lots of the several thousand known rare diseases have overlapping symptoms and the identical disease can appear in a different way in several people. AI tools may also help by examining a patient's unique genetic characteristics and clinical characteristics to find out that are more likely to cause disease. These AI systems can include components that predict whether the patient's specific genetic variation is present has a negative effect on protein function and whether the patient The symptoms are similar to certain rare diseases.
Future of clinical decision making
New technologies will soon make it possible to routinely measure other forms of diseases biomolecular data beyond genetics. Wearable health devices can constantly monitor heart rate, blood pressure and other physiological characteristics and generate data that AI tools can use to diagnose diseases and personalize treatment.
Corresponding studies are already providing promising results Precision oncology and personalized healthcare. For example, researchers are developing one portable ultrasound scanner To detect breast cancer and engineers to develop skin-like sensors to detect changes in tumor size.
The research will proceed to expand our knowledge of genetics, the health effects of environmental exposures, and the way AI works. These developments will significantly change the best way physicians make decisions and deliver care over the subsequent 50 years.
image credit : theconversation.com

















Leave a Reply