Attention: This article comprises graphic images.
When did you first experience xylazine wounds?
Before using xylazine, a lot of the wounds we treated were skin infections akin to abscesses. These conditions occur when a small amount of bacteria gets under the skin and creates an infection site. These infections normally clear up quickly when treated with antibiotics.
At the top of 2019, participants of the wound clinic got here with a unique type of wound. They were full of black and yellow dead tissue and dug deep into the skin. These weren’t wounds brought on by an infection, but by Tissue death or necrosis.
Initially, our clinic patients found that the sores healed on their very own once they switched “brands” of the drug – something like a brand within the unregulated pharmaceutical market. But by the top of 2020, people were experiencing these sores irrespective of what brand they were using.
What was much more disturbing to me and the people I saw on the clinic was the incontrovertible fact that the injuries gave the impression to be appearing on parts of the body where no injections had been given, and even on patients who were snorting or smoking the weed and never injecting it in any respect.

Journal of Addiction Medicine
What causes the injuries?
The medical community doesn't quite understand what causes these wounds. Harm reduction advocates in Puerto Rico published the primary reports on wounds brought on by xylazine greater than a decade ago, and research based on their experience found that the substance direct cytotoxic effectsThis implies that when injected, xylazine kills cells on contact and causes necrotic pockets under the skin.
Xylazine also constricts blood vessels, causes small vessel disease, and lowers heart rate and blood pressure. Together, these effects cause restrict blood flow to the outermost parts of our vascular system – namely our skin and soft tissue. Tissue that doesn’t receive enough oxygen and nutrients as a consequence of this restricted blood supply eventually becomes necrotic and dies. So contact with xylazine by any route, not only injection, can result in small tissue necrosis spread throughout the body and forestall the healing of other skin injuries akin to cuts and bug bites.
Not all scientists are convinced that there’s a causal connection between xylazine and these wounds. For example, I recently attended a lecture on Research panel Meanwhile, one other speaker suggested that a mixture of fentanyl adulterants or the tactic of consumption could also be more more likely to be accountable for the injuries.
I believe this diversity of opinion is nice since it results in more thorough investigations into what is actually happening. But after following the published literature and the evidence that has emerged, and dealing directly with individuals who use drugs, I’m convinced of the connection.
How do you treat them?
There is a helpful mnemonic for wound care – DIME – which I even have adapted barely to summarize a very powerful features of treating these wounds. The D stands for debridement, I for infection and inflammation, M for moisture management and E for environment.
Debridement: Debridement refers back to the removal of dead or necrotic tissue, a typical feature of wounds brought on by xylazine. Healing begins at the underside or deepest a part of the wound, but recent tissue cannot form because layers of dead tissue block the best way. In the clinic, we use ointments that lightly and regularly dissolve the dead tissue. However, large deposits are best removed within the operating room, and sometimes we refer patients to the hospital for this procedure.
Infection and inflammation: On the dead tissue that accumulates in these wounds, every kind of bacteria multiply and form what we a biofilm. Bacterial biofilms nest in and across the necrotic tissue, forming protective capsules which are inaccessible even to intravenous antibiotics. They cause inflammation and might result in infection, each of which delay wound healing. Therefore, we use powerful antimicrobial ointments within the wound that destroy this biofilm, and moreover treat infections with antibiotics once they occur.
Moisture management: Our bodies are 70% water, and in areas without skin where all that fluid might be stored, like these wounds, there’s plenty of drainage. In a xylazine wound, the drainage takes on a foul odor from the necrotic tissue, which is understandably very distressing for those affected. So we frequently see people attempting to dry out their wounds to reduce the mess and odor. But wounds need moisture to heal, so we're working with people within the clinic to develop a wound dressing that keeps the wound bed moist while also directing the drainage in a way that minimizes distress.
Environment: Living on the streets with very limited access to showers, bathrooms or nutritious meals is a reality for many individuals who use fentanyl contaminated with xylazine in Philadelphia. It could be very difficult for people to vary their every day wound dressings when even their Basic needs, including shelter, food and securityare usually not being met. I consider that advocating for resources and policies that address these basic needs is a critical a part of healing these wounds.
Providing prime quality wound care that also takes into consideration the life experiences and realities of drug users is an art and a science. Last 12 months, our Nurse-led clinic published recommendations for the treatment of wounds with xylazine based on our experience with such a treatment in Philadelphia. In January 2024, the Philadelphia Department of Public Health also published a comprehensive recommendations which I highly recommend to anyone who wants to seek out out more.

Spencer Platt/Getty Images
Where can people get treatment?
Few traditional healthcare facilities within the region have addressed the needs of individuals with energetic substance use disorder who require wound care. For example, most outpatient wound care facilities implement strict schedules and sobriety policies. At the identical time, most hospitals provide inadequate pain and withdrawal treatments to patients with fentanyl and xylazine addiction, as evidenced by extremely high Self-discharge rates on this population.
However, there are a handful of low-threshold Wound clinics in Kensington, the North Philadelphia neighborhood that’s the epicenter of the xylazine epidemic. These facilities, where you may receive treatment without an appointment, don’t require insurance or payment and welcome individuals who still use drugs. The city is publishing a schedule for his or her Places and times.
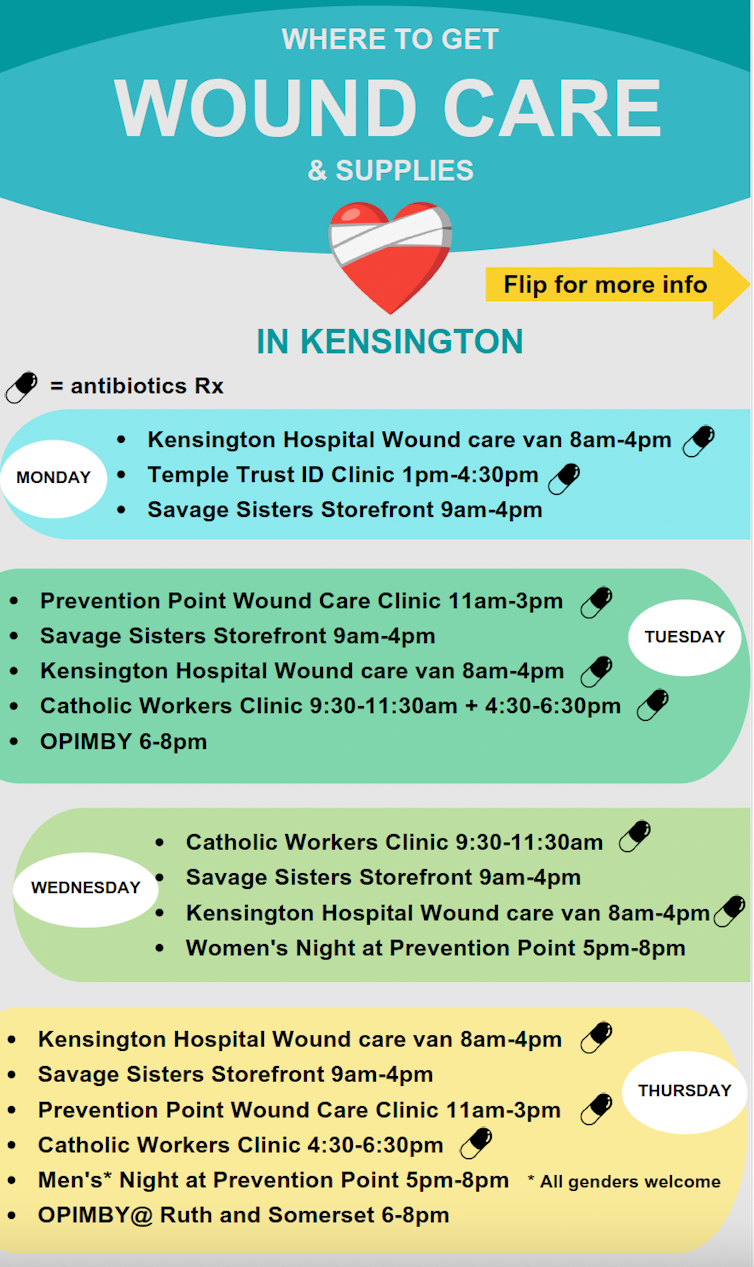
Philadelphia Health Department
But most of those clinics have limited opening hours, operate on very tight budgets, depend on volunteers and donations, and are simply not equipped to supply the care that individuals often need.
How does stigma prevent people from in search of treatment?
It is well documented the stigma of opioid addiction – maintained by Healthcare employees and even from Institutions and politics – can prevent people from from getting the care they need.
For example, researchers at Thomas Jefferson University in Philadelphia found that individuals with wounds brought on by xylazine often refused admission to cleansing and rehabilitation programs until their wound has healed. This also applies in the event that they are medically stable and might deal with their wounds independently.
On the opposite hand, patients who’re being treated for opioid addiction and require advanced medical take care of their wounds are routinely rejected by care facilitiesthat are there to support people, for instance, in wound care.
Our clinic patients have also reported receiving degrading treatment from staff at methadone clinics due to their wounds. And I even have personally observed several cases in Philadelphia where an individual was denied wound care, akin to surgical debridement, due to their drug use.
These barriers to treatment are deeply troubling, and I even have accompanied many hospital patients through emotional moments as they grapple with the injustice of being denied treatment at every turn. I consider that in this crisis, it’s equally essential to supply support and encouragement to people affected by these wounds, while also holding healthcare institutions and systems accountable.
image credit : theconversation.com

















Leave a Reply